ASH 2025 - Washington DC
I am very grateful to HaemSTAR for supporting my trip to Washington, D.C. for ISTH 2025. As this was my first international conference, I arrived not entirely sure what to expect, but it proved to be a genuinely enjoyable and valuable experience.
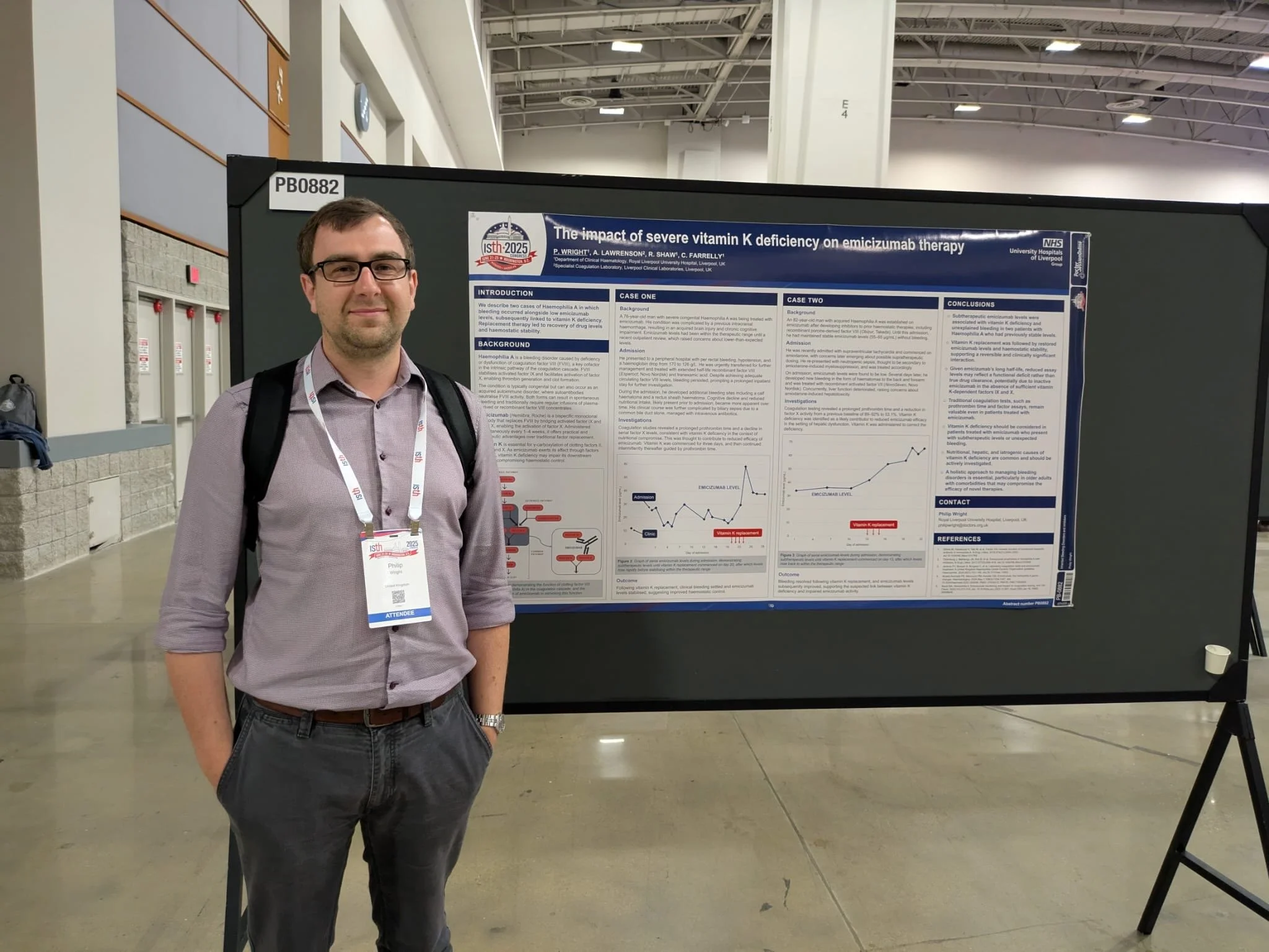
I presented a poster based on a clinical observation we had made about vitamin K deficiency affecting emicizumab effectiveness. I suspected it might be the sort of finding that quietly occupies a corner of the poster hall, so I was pleasantly surprised when several people stopped to discuss it. Many were exploring similar questions in their laboratories, and hearing their perspectives helped me understand where our experience fits within a broader field of work.
The scientific programme was wide ranging, and a few sessions stood out for their immediate clinical relevance. The presentation of the COBRRA data comparing apixaban and rivaroxaban for acute VTE was one of them. The lower rate of clinically important bleeding seen with apixaban, alongside similar efficacy, is exactly the kind of information that feeds into real decisions rather than theoretical debates. It certainly made me think more carefully about how we choose between anticoagulants in different situations.
There was also a short talk on vitamin K dependent pathways that linked neatly back to my poster work. It tied up a few loose ends for me and made the underlying biology feel a little less abstract.
Beyond the formal sessions, the conversations around the conference were just as valuable. Speaking with trainees, clinicians and researchers from different centres gave me a broader sense of how others approach similar challenges. It also made the whole event feel surprisingly welcoming for a meeting of this size.
I came home with practical learning points, a clearer sense of current developments and the feeling that attending in person had genuinely added something to my training. I am very grateful to HaemSTAR for making it possible.